Understanding Particulates in Single-Use Bags
The biopharmaceutical industry is facing many challenges. Global economic changes, increasing
healthcare costs, expiring patents, and increasingly personalized medicine all affect the way
manufacturers approach bioprocessing steps and the equipment and systems used to make biological
drug products (1). Demands for smaller batch sizes, greater process flexibility, reduced manufacturing
costs, and increased speed to clinic have driven the acceptance of single-use systems (SUSs) in this
industry (Figure 1). SUS suppliers have rapidly developed components such as fittings, tubing, pumps,
sensors, and flexible containers that are delivered to users presterilized and ready for use in single
campaigns or process steps.
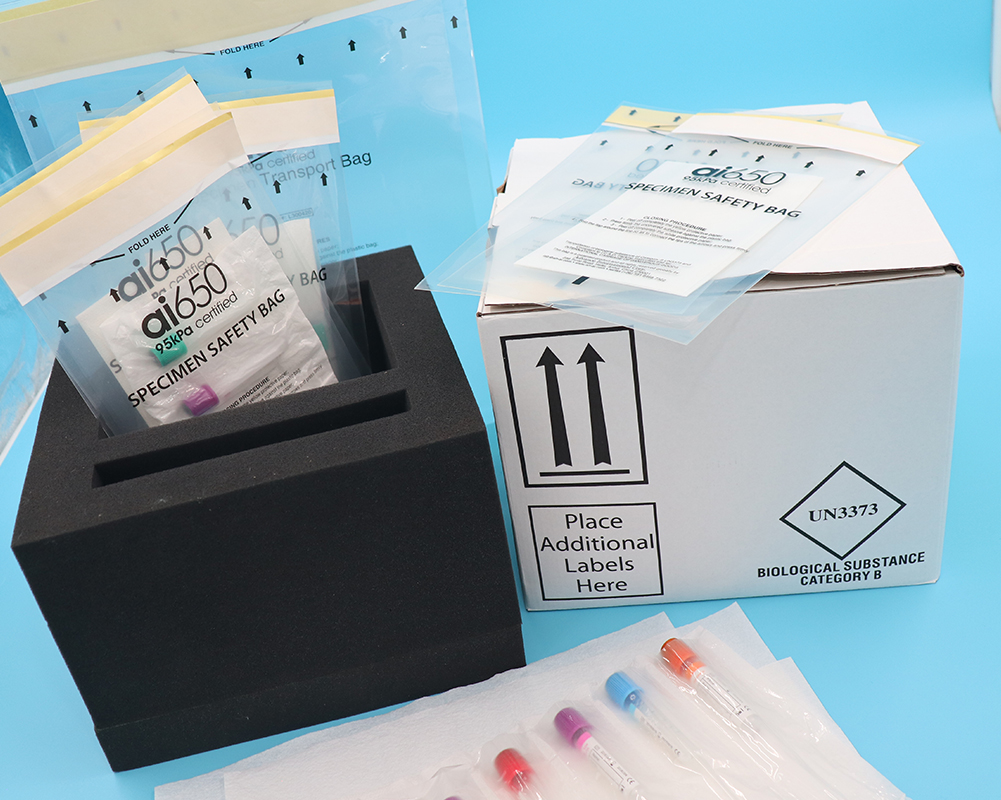
Figure 1:
Applications such as buffer preparation and media storage were the first to adopt single-use components
including filter capsules and plastic biocontainers. As single-use technology became accepted, it moved
into upstream processes with the implementation of disposable bioreactors and mixing systems. The
latest applications of SUSs are in downstream processes such as drug substance storage and final filling .
The benefits of single-use systems have been thoroughly investigated. Some key advantages over
traditional multiuse systems include reductions in capital expenditure; smaller, more flexible
manufacturing footprints; elimination of expensive clean-in-place (CIP) and steam-in-place (SIP)
processes; reduction in cross contamination; and facilitated process changeovers. Along with those
benefits, however, come new areas of concern associated with polymeric materials and disposable
systems.
One area of interest is the cleanliness of SUSs. Because they are intended to be used “as-is,” the
accountability for their cleanliness has shifted from end users to suppliers. Contaminants that are present
in a given system — such as leachable compounds or particulate matter — may be transferred to process
media. Contaminants in upstream SUS processes such as bioreactors and mixing systems pose less risk
because process fluids will be subjected to downstream filtration and purification steps, which could
remove such contaminants from the process stream. The closer SUSs are to final drug products, the
higher the need is to reduce their leachables and particles. Clearly, final process steps such as drug-
substance storage and final filling are high-risk activities that require the lowest levels of leachables and
particulates in SUSs.
Particle Sources
Particulates can come from many different sources. One source is the environment in which a drug
product is manufactured: e.g., heating, ventilation, and air conditioning (HVAC) systems; tools and
equipment used in the facility; and people supporting the manufacturing processes. Components and
used to contain, mix, purify, and transport media throughout such processes present another source of
particles. They include gaskets and seals, vials and syringes, and components making up SUSs such as
tubing, fittings, and bags.
The primary reason to better understand and control particles in SUSs is to reduce their clinical impacts
and ensure patient safety. If infused along with a biologic therapy, particulate matter can block blood
vessels, affecting functional body systems to cause tissue damage and even internal organ failures.
Particles also may be incompatible with a patient’s arterial system, essentially poisoning him or her. Other
potential effects include overtaxation of the immune system and reducing drug efficacy. Factors
determining whether particles in a drug product will affect patients include the size, shape, and quantity
of particles present; the composition of those particles; the dosage, frequency, and route of drug delivery;
and patient attributes such as age and health status (3).
Secondary to the possible clinical impacts are commercial ones. Particulates may contribute to lower
production yields and scrapped batches. The cost of goods sold (CoGS) is also negatively affected,
increasing as the need for more risk-mitigation measures and quality assurance (QA) inspections.
, companies may experience increased scrutiny from regulatory authorities. In one recent incident, 19 lots
of drug product were recalled because of glass particles found in vials (4). That occurred even after
several warning letters were issued by the US Food and Drug Administration (FDA) and expensive
upgrades were completed for multiple facilities (4).
In an ongoing effort to mitigate particles, several regulatory groups have developed standards that are
continually reviewed and updated by those same groups. Table 1 is a partial list of such standards. One
commonly referenced standard is USP Chapter <788>, which establishes methods to quantify particles
and provides acceptable limits for particulates in injections. Limits established in USP Chapter <788>
depend on the method used (light obscuration or microscopic particle count) and whether a sample
comes from a large-volume (>100 mL) or small-volume (≤ 100 mL) parenteral dose. Figure 2 lists those
limits


No responses yet